CASES OF THE WEEK – “A Case of recurrent Conjunctivitis & Blocked Tear Duct - The role of Lacrimal Duct Scintigraphy (Dacryocystography)” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine
A Case of recurrent Conjunctivitis & Blocked Tear Duct - The role of Lacrimal Duct Scintigraphy (Dacryocystography)
Introduction
When you have a blocked tear duct, your tears can't drain normally, leaving you with a watery, irritated eye. The condition is caused by a partial or complete obstruction in the tear drainage system.
A blocked tear duct is common in newborns. The condition usually gets better without any treatment during the first year of life. In adults a blocked tear duct may be due to an injury, an infection or a tumor. A blocked tear duct is almost always correctable. Treatment depends on the cause of the blockage and the age of the affected person.
The lacrimal glands produce most of your tears. These glands are located inside the upper lids above each eye. Normally, tears flow from the lacrimal glands over the surface of your eye. Tears drain into the puncta, located in the inside corners of your upper and lower eyelids.
Your eyelids have small canals (canaliculi) that move tears to a sac where the lids are attached to the side of the nose (lacrimal sac). From there tears travel down a duct (the nasolacrimal duct) draining into your nose. Once in the nose, tears are reabsorbed.
A blockage can occur at any point in the tear drainage system, from the puncta to your nose. When that happens, your tears don't drain properly, giving you watery eyes and increasing your risk of eye infections and inflammation.
Symptoms
Signs and symptoms of a blocked tear duct include:
- Excessive tearing
- Redness of the white part of the eye
- Recurrent eye infection or inflammation (pink eye)
- Painful swelling near the inside corner of the eye
- Crusting of the eyelids
- Mucus or pus discharge from the lids and surface of the eye
- Blurred vision
Causes
Blocked tear ducts can happen at any age. They may even be present at birth (congenital). Causes include:
- Congenital blockage. Many infants are born with a blocked tear duct. The tear drainage system may not be fully developed or there may be a duct abnormality. Often a thin tissue membrane remains over the opening that empties into the nose (nasolacrimal duct).
- Age-related changes. As you age, the tiny openings that drain tears (puncta) may get narrower, causing blockage.
- Infection or inflammation. Chronic infection or inflammation of your eyes, tear drainage system or nose can cause your tear ducts to become blocked.
- Injury or trauma. An injury to your face can cause bone damage or scarring near the drainage system, disrupting the normal flow of tears through the ducts. Even small particles of dirt or loose skin cells lodged in the duct can cause blockage.
- Tumor. A tumor in the nose or anywhere along the tear drainage system can cause blockage.
- Inflammatory conditions. Disorders that cause swelling, such as sarcoidosis or granulomatosis with polyangiitis, can increase the risk of developing a blocked tear duct.
- Eye-drops. Rarely, long-term use of certain medications, such as eye-drops used to treat glaucoma, can cause a blocked tear duct.
- Cancer treatments. A blocked tear duct is a possible side effect of chemotherapy medication and radiation treatment for cancer.
Complications
Tears aren't draining the way they should, the tears that remain in the drainage system become stagnant. This promotes growth of bacteria, viruses and fungi, which can lead to recurrent eye infections and inflammation.
Any part of the tear drainage system, including the clear membrane over your eye surface (conjunctiva), can become infected or inflamed because of a blocked tear duct.
Case
44 years old lady with history of recurrent right eye infection (conjunctivitis) each year since long (2010). Complaining of right watery eye and nasal blockage since last five months.
Underwent nasolacrimal intubation but no obvious relief and hence referred for ENT work up, which was unremarkable.
Referred of Lacrimal Duct Scintigraphy (Dacryocystography)
99m Technetium Pertechnetate Dacryocystography
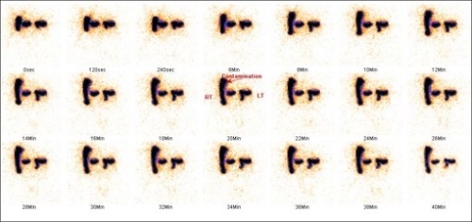
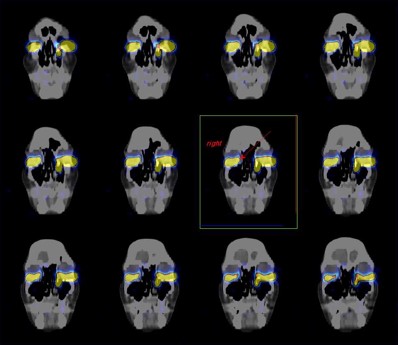
Dynamic images of both eyes were obtained in anterior supine position for the period of 40 minutes and subsequently static images are obtained at 45 min and SPECT-CT fused images at 120 min
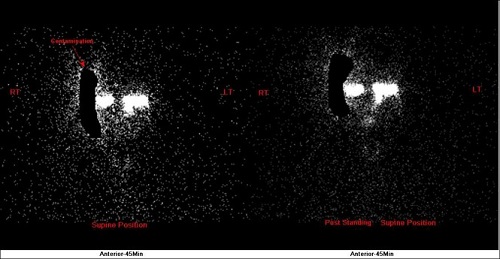
Left eye shows physiological tracer excretion into nasal cavity with well visualization of whole of the lacrimal duct.
Right eye shows physiological obstructive flow pattern at the level of punctum (As shown with arrow on SPECT-CT FUSED images).
The diagnosis of a right eye punctum stenosis was made.
Procedure
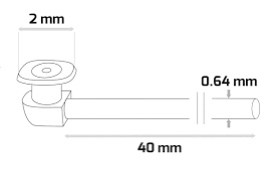
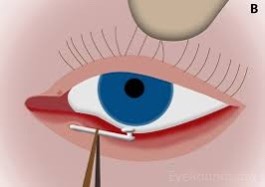
A 3-snip punctum opening was performed and a mini-Monaco tube was intubated to keep the punctum open and allow the tear to enter the lacrimal canal and thus her epiphora is controlled.
Conclusion
Lacrimal scintigraphy evaluates the lacrimal drainage apparatus in a “physiological” manner, that is, with pressure gradients present in every-day life; thus, it may be more suitable for the study of functional epiphora than other imaging modalities.



