CASES OF THE WEEK – “Use of Sentinel Node Lymphoscintigraphy in Malignant Melanoma” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine, Dr Nadeem Akhtar, HOD & Consultant, Plastic Surgery, Dr Ehsan Ahmed, Specialist, Clinical Pathology
Use of Sentinel Node Lymphoscintigraphy in Malignant Melanoma
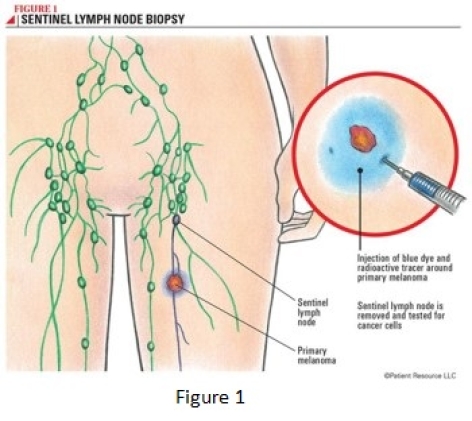
Lymphoscintigraphy is used to track how malignant cells travel in lymph channels throughout the body. The lymph vessels that carry malignant cells follow patterns and trails yet are still unique to each type of malignancy.
The SLN is the nodal site of potential micro metastasis. SLNs are the main focus of lymphoscintigraphy because these nodes indicate where malignant cells will spread first. This knowledge defines the route of potential treatment and the prognosis for melanoma patients. The presence of regional lymph node involvement is the single most important prognostic factor. Assessing how far the tracer has traveled also indicates how far the malignancy has traveled. SLNs are the first draining node in the lymphatic chain. These chains are normal free-flowing channels throughout the entire body. By identifying the SLN, or where the lymph fluid travels first in the body, one can map the route of the malignancy. The presence of an SLN on lymphoscintigraphy images does not indicate that a malignancy has been found. But by locating this node, surgeons can remove it and send a sample to be tested for malignancy.
Lymphoscintigraphy assesses obstruction, flow, and malignancy in lymph nodes. The theory of lymph node mapping entails injecting a radioactive tracer and performing imaging to follow the route of the tracer, determine where it builds up, and see how far it can travel. Lymphoscintigraphy relies on the SLN and lymphatic channels in the individual patient. There are thousands of cellular and physical differences between human beings. Malignancies that travel in lymph channels are among the most dangerous, and the exact placement of every SLN varies between individuals. Regionally, lymph nodes are typically found in standard areas from patient to patient. This standardized, regional flow gives the familiar patterns in which SLNs are commonly found; however, discovery of abnormal SLNs is not unusual.
The radiopharmaceutical injection relies on the lymphatic system’s ability to transport large molecules from the interstitial spaces back to the vascular system and the tracer used 99mTc Nano Colloid (Small particles <100 nm) clears from the interstitial spaces, (<37 MBq [1 mCi]), the radiation dose to the patient is often considered insignificant.
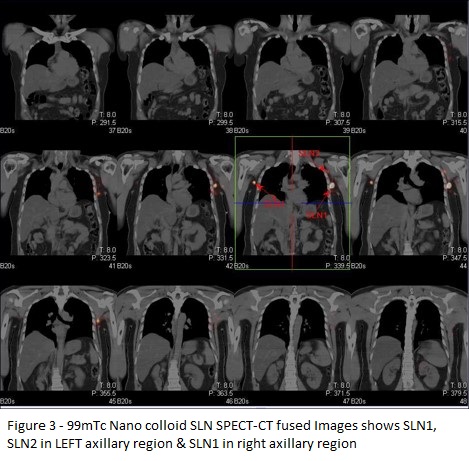
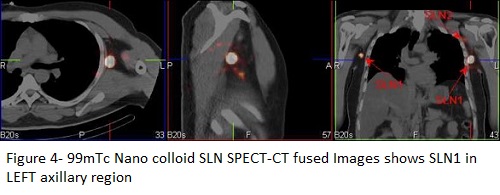
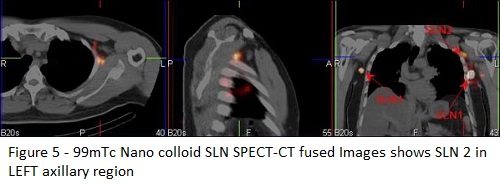
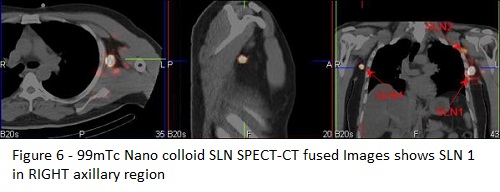
SPECT/CT (single-photon emission computed tomography) provides corresponding functional and anatomical details, good contrast resolution and has proven superiority over planar imaging under various conditions as it overcomes limitations of PS The combination of a SPECT camera and a “low dose CT “ postulates a useful map for the surgeon facilitating surgical exploration and is especially useful in unveiling “hot” nodes not seen on PS, eliminates sites of false-positive uptake sites and accurately pinpoints axillary and extra axillary hot nodes. Attenuation and scatter correction has led to superior SLN identification.
Case
41 years old gentleman with three to four months history of rapid swelling and darkening lesion to the left lower back along with itching. Punch biopsy confirmed Malignant Melanoma. On examination- four to five centimeter in diameter, irregular edged large lesion on the left thoracic back close to the midline with no deeper fixating, no axillary nor inguinal nodes palpable bilaterally.
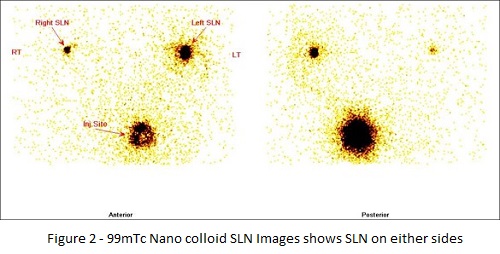
99mTc – Nano colloid SENTINEL LYMPH NODE SCINTIGRAPHY
Sentinel lymph nodes are seen in both sides of axillary region
Left axilla a) bigger one SLN1 with avid tracer uptakes and adjacent to this smaller one SLN2 with less avid tracer uptakes and it is in mid axillary region approximately.
Right axilla-smaller one with less avid tracer uptakes and it is in mid axillary region approximately.
Subsequently underwent wide excision of malignant melanoma ( left lower thoracic region). HP- Lentigo malignant melanoma, tumor sise 4.5 cms ( horizontal growth), tumor Breslow thickness 1.9mm, lymphovascular invasion probable, anatomic clarks level 4, deep margin free from tumor, ( T2a,N1a sn).
Gamma probe guides sentinel lymph node removal
SLN1 ( left axillary region ) - Consistent with microm metastatic melanoma and the tumor deposit measures 1.4 mm.
SLN2 ( LEFT AXILLARY REGION ) – NEGATIVE FOR METSTATIC TUMOR, SHOWING NON SPEIFIC REACTIVE HYPERPLASIS.
SLN1 ( RIGHT AXILLA ) NEGATIVE FOR METSTATIC TUMOR, SHOWING NON SPEIFIC REACTIVE HYPERPLASIS.
SPECT/CT (single-photon emission computed tomography) provides corresponding functional and anatomical details, good contrast resolution and has proven superiority over planar imaging under various conditions as it overcomes limitations of PS The combination of a SPECT camera and a “low dose CT “ postulates a useful map for the surgeon facilitating surgical exploration and is especially useful in unveiling “hot” nodes not seen on PS, eliminates sites of false-positive uptake sites and accurately pinpoints axillary and extra axillary hot nodes. Attenuation and scatter correction has led to superior SLN identification.
Case
41 years old gentleman with three to four months history of rapid swelling and darkening lesion to the left lower back along with itching. Punch biopsy confirmed Malignant Melanoma. On examination- four to five centimeter in diameter, irregular edged large lesion on the left thoracic back close to the midline with no deeper fixating, no axillary nor inguinal nodes palpable bilaterally.
99mTc – Nano colloid SENTINEL LYMPH NODE SCINTIGRAPHY
Sentinel lymph nodes are seen in both sides of axillary region
Left axilla a) bigger one SLN1 with avid tracer uptakes and adjacent to this smaller one SLN2 with less avid tracer uptakes and it is in mid axillary region approximately.
Right axilla-smaller one with less avid tracer uptakes and it is in mid axillary region approximately.
Subsequently underwent wide excision of malignant melanoma ( left lower thoracic region). HP- Lentigo malignant melanoma, tumor sise 4.5 cms ( horizontal growth), tumor Breslow thickness 1.9mm, lymphovascular invasion probable, anatomic clarks level 4, deep margin free from tumor, ( T2a,N1a sn).
Gamma probe guides sentinel lymph node removal
SLN1 ( left axillary region)-Consistent with microm metastatic melanoma and the tumor deposit measures 1.4 mm.
SLN2 ( LEFT AXILLARY REGION – NEGATIVE FOR METSTATIC TUMOR, SHOWING NON SPEIFIC REACTIVE HYPERPLASIS.
SLN1 ( RIGHT AXILLA) NEGATIVE FOR METSTATIC TUMOR, SHOWING NON SPEIFIC REACTIVE HYPERPLASIS.
CONCLUSION
Lymphoscintigraphy is a sensitive, inexpensive, relatively noninvasive method of identifying lymphatic drainage patterns and sentinel lymph nodes in patients with malignant melanoma. Lymphoscintigraphy with filtered technetium-99m sulfur colloid allows prompt visualization of the lymphatic system, produces high-quality images, and delivers a low radiation dose to the patient. In addition, good regional lymph node retention is seen with filtered Tc-99m sulfur colloid, improving the success rate of intraoperative gamma probe localization. In combination with surgical localization, lymphoscintigraphy allows preoperative and intraoperative identification of the sentinel node in patients with intermediate thickness melanomatous lesions, obviating radical lymph node dissection in most patients and possibly prolonging their survival. Variables such as tumor location, type and preparation of radiopharmaceutical, injection technique, imaging technique, and prior surgical intervention influence the efficacy of lymphoscintigraphy. Nevertheless, lymphoscintigraphy is recommended as a cost-effective preoperative procedure in all patients planning to undergo elective lymph node dissection. Because of the unpredictability of lymphatic drainage, preoperative scintigraphic findings may lead to changes in surgical management.
Lymphoscintigraphy is a sensitive, inexpensive, relatively noninvasive method of identifying lymphatic drainage patterns and sentinel lymph nodes in patients with malignant melanoma. Lymphoscintigraphy with filtered technetium-99m sulfur colloid allows prompt visualization of the lymphatic system, produces high-quality images, and delivers a low radiation dose to the patient. In addition, good regional lymph node retention is seen with filtered Tc-99m sulfur colloid, improving the success rate of intraoperative gamma probe localization. In combination with surgical localization, lymphoscintigraphy allows preoperative and intraoperative identification of the sentinel node in patients with intermediate thickness melanomatous lesions, obviating radical lymph node dissection in most patients and possibly prolonging their survival. Variables such as tumor location, type and preparation of radiopharmaceutical, injection technique, imaging technique, and prior surgical intervention influence the efficacy of lymphoscintigraphy. Nevertheless, lymphoscintigraphy is recommended as a cost-effective preoperative procedure in all patients planning to undergo elective lymph node dissection. Because of the unpredictability of lymphatic drainage, preoperative scintigraphic findings may lead to changes in surgical management.