CASES OF THE WEEK – “Sentinel Lymph Node (Sln) Scintigraphy in Primary Mucinous Carcinoma of the Scalp” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine, NMC Royal Hospital Sharjah
SENTINEL LYMPH NODE (SLN) SCINTIGRAPHY IN PRIMARY MUCINOUS CARCINOMA OF THE SCALP
Mucinous sweat gland carcinoma is a rare malignant tumor of the skin. We report herein the case of a 42-year-old lady who presented with a scalp mass. Primary cutaneous mucinous carcinoma is a rare adnexal sweat gland neoplasm that mainly affects elderly people. Differential diagnosis includes mammary and gastrointestinal metastatic mucinous carcinoma (MC) and secondary cutaneous involvement by underlying neoplasms.
Case
A 42-years-old lady underwent excision of a tender scalp swelling (sub cutaneous mass) over left occipital scalp region close to midline.
Histopathological examination of the mass revealed mucinous carcinoma. Extensive metastatic work-up, including a total body computed tomographic and positron emission scan (Whole body PET/CT scan), showed
No evidence of FDG avid focal lesion in the scalp.
No evidence of FDG avid lymph adenopathy.
No evidence of FDG avid distant/organ deposit.
Incidental findings- bilateral maxillary sinusitis, mild hepatomegaly and mild dorso-lumbar spondylosis.
Referred for SENTINEL LYMPH NODE SCINTIGRAPHY
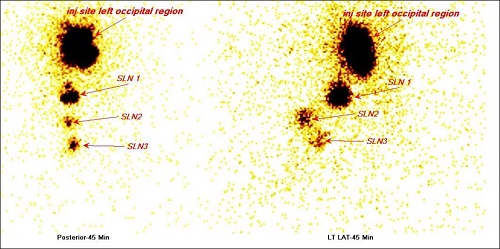
99m Tc – NC SENTINEL LYMPH NODE SCINTIGRAPHY
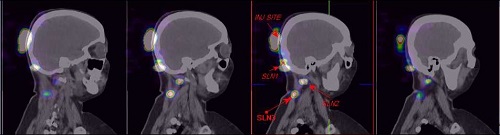
Sentinel lymph nodes are seen in Left occipital region (SLN1)- shown with arrow.
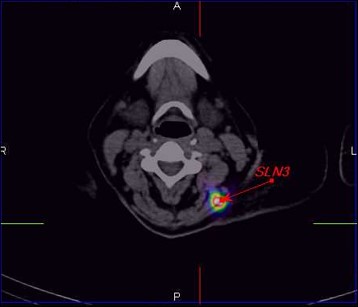
Left upper deep cervical lymph nodes (SLN2 and SLN3) shown with arrow.
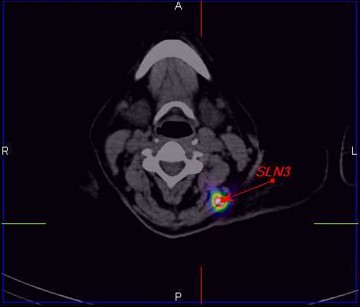
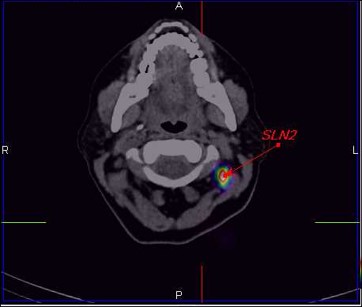
Through Gamma probe guided sentinel lymph nodes were localised and removed. Histopathology shows negative for micro-metastasis.
Lymphoscintigraphy is used to track how malignant cells travel in lymph channels throughout the body. The lymph vessels that carry malignant cells follow patterns and trails yet are still unique to each type of malignancy.
The SLN is the nodal site of potential micro metastasis. SLNs are the main focus of lymphoscintigraphy because these nodes indicate where malignant cells will spread first. This knowledge defines the route of potential treatment and the prognosis for melanoma patients. The presence of regional lymph node involvement is the single most important prognostic factor. Assessing how far the tracer has traveled also indicates how far the malignancy has traveled. SLNs are the first draining node in the lymphatic chain. These chains are normal free-flowing channels throughout the entire body. By identifying the SLN, or where the lymph fluid travels first in the body, one can map the route of the malignancy. The presence of an SLN on lymphoscintigraphy images does not indicate that a malignancy has been found. But by locating this node, surgeons can remove it and send a sample to be tested for malignancy.
SPECT/CT (single-photon emission computed tomography) provides corresponding functional and anatomical details, good contrast resolution and has proven superiority over planar imaging under various conditions as it overcomes limitations of PS The combination of a SPECT camera and a “low dose CT “ postulates a useful map for the surgeon facilitating surgical exploration and is especially useful in unveiling “hot” nodes not seen on PS, eliminates sites of false-positive uptake sites and accurately pinpoints hot nodes. Attenuation and scatter correction have led to superior SLN identification.
CONCLUSION
Primary mucinous eccrine carcinoma has a local recurrence rate greater than 36% after surgical excision. Patients should be seen for skin examination at least twice a year and educated in self-skin examination to look for local recurrence and possible regional lymphadenopathy.



