CASES OF THE WEEK – “Rifamipicin induced uncontrolled Hypertension in CKD patient” by Dr Aditya Bhabhe, Consultant, Nephrology & Dr Salahudeen Fizal, Specialist, Pulmonology
Rifamipicin induced uncontrolled Hypertension in CKD patient
A 50-year-old male patient is a known case of Hypertension, Diabetes Mellitus and Coronary Artery disease. He also has CKD stage 5D and is on regular hemodialysis twice a week since the past 2 years.
The patient was receiving 4 classes of antihypertensive medications: Calcium channel blockers; ARB; alpha-blockers and Beta-blockers. This is not very unusual in patients on dialysis and his blood pressure was reasonably well controlled.
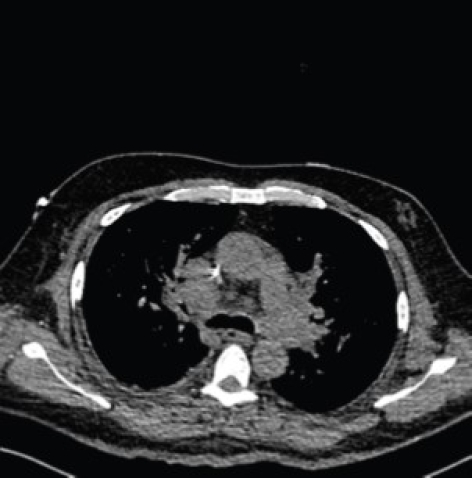
He was admitted to the hospital with complaints of fever cough and dyspnea. CT scan showed multiple enlarged thoracic and abdominal lymph nodes. Biopsy of the nodes was suggestive of Tuberculosis. In consultation with Pulmonologist, the patient was started on Intensive phase treatment of Tuberculosis as per WHO/ CDC guidelines. The medicines included Isoniazid; Rifampicin; Ethambutol and Pyrazinamide in renally adjusted doses.
Within one week of starting ATT, the patient started complaining of uncontrolled hypertension. His antihypertensive medications were progressively increased.
After 2 weeks, he was on double the maximum doses of Amlodipine; Moxonidine; Olmesartan; Hydralazine; Prazosin; Lasix and Bisoprolol. Inspite of such intensive antihypertensive treatment; his blood pressure was severely elevated in the range of 240/120 mm Hg
At this point we decided to with hold his Rifampicin as it is known to be a potent inducer of drug metabolism via Hepatic cytochrome P450. Rifamipicin was substituted by Levofloxacin.
Within 5 days of this change of medications, patient’s blood pressure was within normal range and he was back to his usual anti hypertensive medicine regime.
Conclusion:
Patients on dialysis have an increased incidence of tuberculosis (TB). Rifampicin, a first-line antitubercular therapy (ATT) drug, is a potent inducer of hepatic cytochrome P450 (CYP). There is potential for pharmacokinetic interaction between rifampicin and anti-hypertensives that are CYP substrates: especially Calcium channel blockers; Beta blockers and alpha blockers. Therefore, hypertensive patients receiving rifampicin-based ATT are at risk for worsening of hypertension and this interaction should be thought of in similar case scenarios. It would be prudent to monitor patients closely for worsening of hypertension after initiation of rifampicin and sometimes we may need to use an alternative antitubercular drug in place of rifampicin.



