CASES OF THE WEEK – “Osteitis Fibrosa Cystica of olecranon process of left ulnar bone, as Initial Manifestation of Primary Hyperparathyroidism” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine
Abstract
Primary hyperparathyroidism is disease of excessive secretion of parathyroid hormone. Osteitis fibrosa cystica or brown tumor, complication of primary hyperthyroidism is characterized by fibrotic cystic bony changes. Skeletal manifestations in the form of brown tumors are rare occurring less than 2% of patients suffering from any form of hyperparathyroidism. We report a 45-year-old woman with lytic expansile lesions in olecranon process of left ulnar bone, diagnosed as osteitis fibrosa cystica secondary to large sized parathyroid adenoma.
Herewith we report a case with primary hyperparathyroidism caused by parathyroid adenoma presented with osteitis fibrosa cystica of olecranon process of left ulnar bone, unusual first manifestation of the disease process.
Introduction
Osteitis fibrosa cystica (OFC) is a skeletal disorder caused by a surplus of parathyroid hormone (PTH) from overactive parathyroid gland (s). This surplus stimulates the activity of osteoclasts, cells that breakdown bone. The overactivity of the parathyroid glands (primary hyperparathyroidism) can be triggered by parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Majority of hyperparathyroidism is the result of parathyroid adenoma (80–85%). The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood and include bone fractures, kidney stones, nausea, peptic ulcers, appetite loss, and weight loss— “bones, stones, abdominal groans and psychic overtones”. Women are more often affected than men, and it occurs more frequently in the 5th and 6th decades. If it occurs in the younger (especially first decade), rule out hereditary causes—multiple endocrine neoplasia type I/IIa/IIb . The serum calcium (8.4–10.2 mg/dL), PTH (15–65 pg/mL), and alkaline phosphatase (20–140 IU/L) are usually elevated. Plain radiographs distinctly show resorption, and the skull depicts the “ground glass”/“salt and pepper” appearance. The first bones to show X-ray features are the fingers. The cysts are lined by osteoclasts and sometimes blood pigments, which lend to the notion of “brown tumors”; such cysts can be identified with nuclear imaging combined with specific tracers, such as Sestamibi.
Case report
A 40-years-old lady presented with complaining of pain and swelling in the left elbow since last 8 to 9 months, which was slowly progressive in nature. CT scan of left elbow demonstrated expansile lytic lesion of the olecranon process of ulna, showing central hypodensity and thick shell of calcification at the margins & lesion has poor zone of demarcation from the adjacent shaft of the ulna (fig 1,2,3) and suspected to be high probability of browns tumor.
The biochemical investigations showed elevated serum calcium levels of 13.3 mg/dL (normal 8.5-10.5 mg/dL), serum phosphorus of 1.6 mg/dL (normal 2.7-4.5 mg/dL) and serum parathyroid hormone of 1002.20 pg/mL (normal up to 11.5 pg/mL) and the renal profile were normal.
Ultrasound scan of neck showed a well-defined hypoechoic lesion at inferior third portion of right lobe of thyroid with increased vascularity. A possibility of right inferior parathyroid adenoma was suggested.
99m Tc-MIBI Parathyroid Scintigraphy (Static early & delayed images and early SPECT CT fused & whole body images) showed focal large area of abnormal MIBI tracer accumulation (4.1*2.1 centimeter in size approximately) in inferior-posterior portion of right lobe on initial whole body, static and delayed washout images (fig 4,9) and well defined anatomically and physiologically on early SPECT CT fused images(fig 5,6,7,9)
In addition to this there is mixed abnormal MIBI tracer accumulation (i.e., uptakes seen medially, and no uptakes seen laterally) seen in olecranon process tumor region of left ulna on whole body and static spot images (fig 8,9)
Based on the above findings the diagnosis of primary hyperparathyroidism with osteitis fibrosa cystica (Brown Tumor) due to large sized parathyroid adenoma was made. Right inferior parathyroidectomy was done, and the histopathological examination confirmed the lesion as parathyroid adenoma. Two weeks postoperatively, the serum levels of calcium and parathyroid hormone declined to their normal limits.
Discussion
Osteitis fibrosa cystica was first reported and described in the nineteenth century (1891) by von Recklinghausen in 1891; it presents as the end stage findings of hyperparathyroidism. Before 1950, around a half of those diagnosed with hyperparathyroidism in the United States saw it progress to OFC, but with technical development of imaging and laboratory screening methods, hypercalcemia due to primary or secondary hyperthyroidism can be detected early :as a result instances of OFC in developed countries are increasing rare.
The high visibility of primary hyperparathyroidism in the population today marks a dramatic change from several generations ago when it was considered a rare disorder . The increase in incidence is primarily due to widespread use of the autoanalyzer gratuitously providing serum calcium determination when a serum chemistry profile is ordered for another reason . Where treatment is required, it entails addressing the underlying hyperparathyroidism before commencing long-term treatment for OFC.
Primary hyperparathyroidism is characterized by the hyperfunctioning of parathyroid glands. The female: male ratio is 5:2. About 85% of cases are caused by a sporadic PTH secreting solitary adenoma of parathyroid chief cells. Multiglandular parathyroid hyperplasia occurs in 1-15% of patients with primary hyperparathyroidism. Parathyroid carcinoma is rare and occurs in less than 1% of cases. Although this condition can occur at any age, it commonly affects people over the age of 50 years and postmenopausal women. Excessive secretion of PTH causes bone resorption accompanied by fibrovascular marrow replacement and increased osteoblastic activity; the imbalance of osteoclastic and osteoblastic activity manifest as a slow enlarging painful bony mass, osteitis fibrosa cystica, which can lead to pathological fractures. The imaging studies, high serum calcium and PTH levels are useful for diagnosis. Treatment of osteitis fibrosa cystica caused by primary hyperparathyroidism is surgical removal of the parathyroid adenoma.
This patient represents what was experienced in the developed countries before the 50s. The successful parathyroidectomy resulted in disease cure.
Osteitis Fibrosa Cystica of olecranon process of left ulnar bone, as Initial Manifestation of Primary Hyperparathyroidism


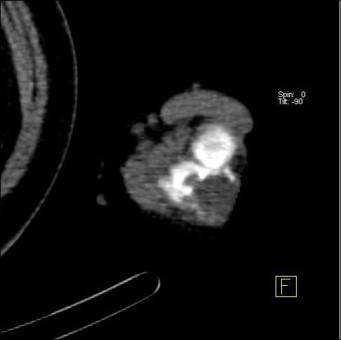
CT SCAN IMAGES OF LEFT ELBOW JOINT
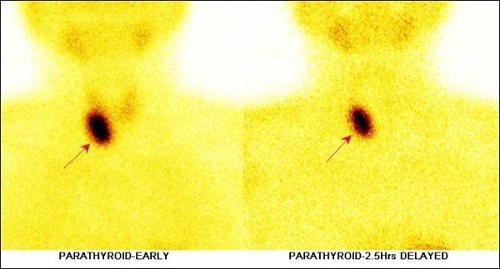
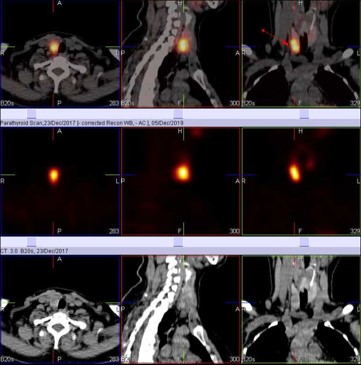
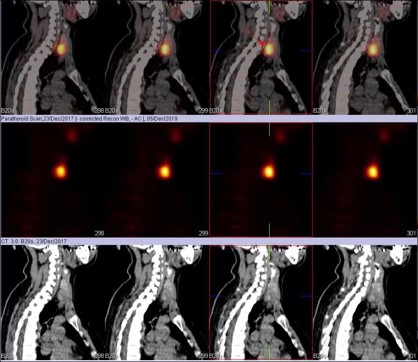
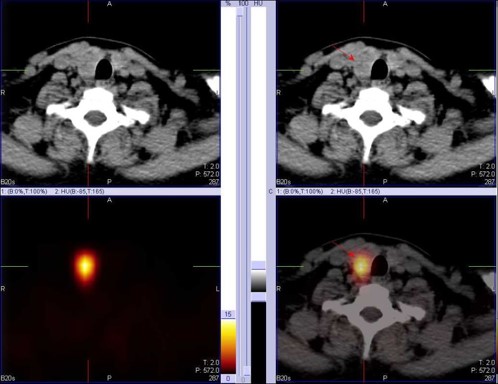
99m Tc-MIBI Parathyroid Scintigraphy (Static early & delayed images and early SPECT CT fused & whole body images) showed focal large area of abnormal MIBI tracer accumulation (4.1*2.1 centimeter in size approximately) in inferior-posterior portion of right lobe on initial whole body, static and delayed washout images and well defined anatomically and physiologically on early SPECT CT fused images
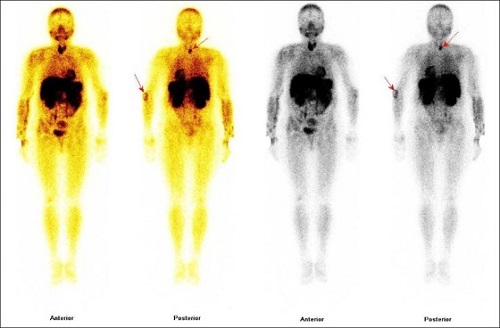
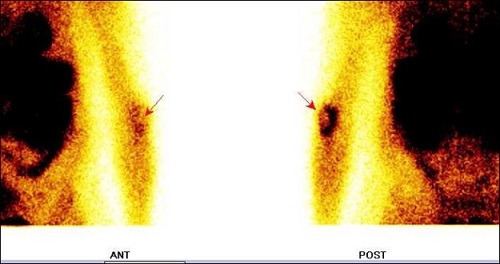
In addition to this there is mixed abnormal MIBI tracer accumulation (i.e., uptakes seen medially, and no uptakes seen laterally) seen in olecranon process tumor region of left ulna on whole body and static spot images



