CASES OF THE WEEK - “Nuclear medicine imaging of myocardial viability & its practical implication” by Dr ShekharShikare, Consultant & HOD, Nuclear Medicine, NMC Royal Hospital Sharjah
Nuclear medicine imaging of myocardial viability & its practical implication
Definition of Myocardial Viability
“Stunned myocardium” results from a rapid, severe episode of coronary occlusion followed by recovery of coronary flow. An abrupt decrease in coronary flow causes contractile dysfunction, which persists even after its restoration. Despite minimal necrosis, ventricular dysfunction may be prolonged, from hours or even weeks. The repeated episodes of ischemia may lead to cumulative stunning, which contributes to the development of chronic, post-ischemic, left ventricular dysfunction. Interestingly, similar degrees of left ventricular dysfunction in distinct patients may be associated with significant differences in the degree of myocardial viability.
Besides, viability is not correlated with myocardial wall thickness, since ventricular wall thinning does not necessarily mean absence of myocardial viability. Hibernating myocardium” has been defined as the presence of severe systolic dysfunction with evidence of hypoperfusion at rest; it refers to a myocardium with preserved cellularity, but reduced blood flow, leading to depressed ventricular function, even at rest. The first theory of hibernating myocardium characterized it as an adaptation to chronic hypoperfusion whose intensity was not sufficiently significant to cause infarction. Hibernating is also known to have intrinsic cellular and extracellular changes, that may be associated with the time required for reversibility of the process, which may vary from days to 14 months.
Determination of myocardial viability is a common and clinically relevant challenge, that may be necessary in post-infarction patients receiving thrombolytic therapy. Also, it may be helpful for surgeons and cardiologists in choosing the best therapy from interventionist strategy, angioplasty and myocardial revascularization.5 This is particularly important in cases when myocardial revascularization is considered, due to high mortality rate and perioperative morbidity in these patients.
THALLIUM-201 IMAGING TO ASSESS MYOCARDIAL VIABILITY.
Cellular viability requires intact sarcolemma function to maintain electrochemical gradients across the cell membrane and preserved metabolic activity to generate high-energy phosphates. These processes require adequate myocardial blood flow to deliver substrates and washout metabolites.
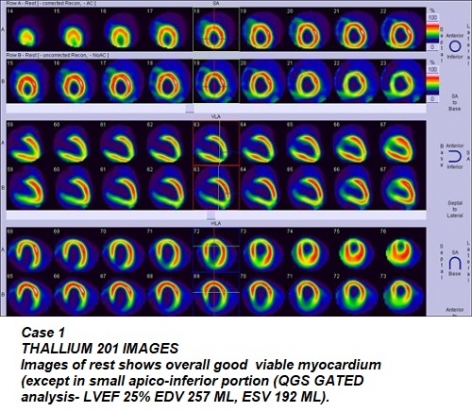
Case 1
49 years old male positive history of progressive dyspnea and orthopnea for one year associated with chest discomfort. History of HTN since many years and on medications. 2D Echo showed four chambers enlargement, LVEF 25%, Moderate to sever MR, Moderate TR, Moderate to sever pulmonary HTN. X ray chest showed global heart enlargement with no obvious signs of pulmonary edema.
Referred for Thallium 201 scan for the myocardial viability to decide about revascularization.
THALLIUM 201 SCAN REST IMAGES SHOWS (QGS GATED ANALYSIS overall good viable myocardium (except in small apicoinferior portion -(QGS GATED analysis- LVEF 25% EDV 257 ML, ESV 192 ML).
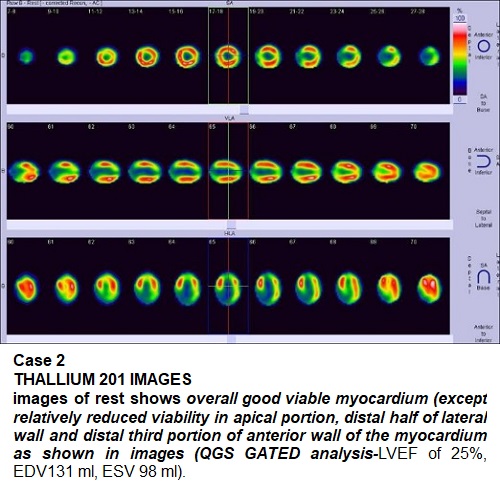
Case 2
67 years old male with history of progressive dyspnea with on and off chest heaviness. 2D Echo- dilated LV, LVEF 25% with global hypokinesia. History of HTN and DM for many years. Referred for Thallium 201 scan for the myocardial viability to decide about revascularization
THALLIUM 201 SCAN REST IMAGES SHOWS overall good viable myocardium (except relatively reduced viability in apical portion, distal half of lateral wall and distal third portion of anterior wall of the myocardium as shown in images (QGS GATED analysis-LVEF of 25%, EDV131 ml, ESV 98 ml).
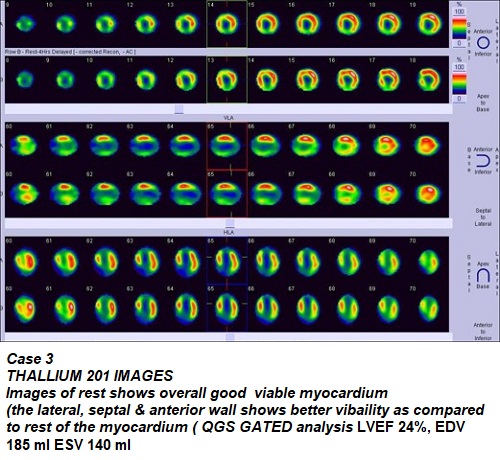
Case 3
68 years old male with history of shortness of breath with small exertion with chest heaviness. 2D echo- dilated LV, LVEF 23% with global hypokinesia. history of long standing HTN & LIPEDIMEIA.
Referred for Thallium 201 scan for the myocardial viability to decide about revascularization
THALLIUM 201 SCAN REST IMAGES SHOWS overall good but variable viable myocardium (the lateral, septal & anterior wall shows better viability as compared to rest of the myocardium (QGS GATED analysis LVEF 24%, EDV 185 ml ESV 140 ml
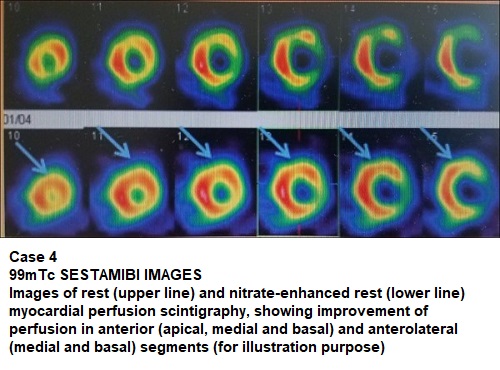
Case 4
99mTc SESTAMIBI IMAGES Images of rest (upper line) and nitrate-enhanced rest (lower line) myocardial perfusion scintigraphy, showing improvement of perfusion in anterior (apical, medial and basal) and anterolateral (medial and basal) segments (for illustration purpose)
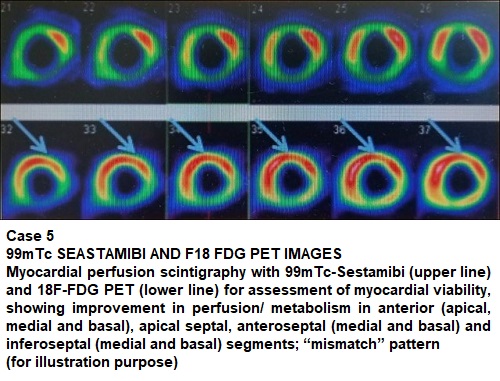
Case 5
99mTc SEASTAMIBI AND F18 FDG PET IMAGES Myocardial perfusion scintigraphy with 99mTc-Sestamibi (upper line) and 18F-FDG PET (lower line) for assessment of myocardial viability, showing improvement in perfusion/ metabolism in anterior (apical, medial and basal), apical septal, anteroseptal (medial and basal) and inferno-septal (medial and basal) segments; mismatch” pattern (for illustration purpose)
F18 FDG PET is the gold standard (100% approximately) for the evaluation of myocardial viability. however, in absence of PET, THALLIUM2 201 scan will be the next ideal imaging of the choice (85 to 90% approximately) & the last but not the least is 99mTc Sestamibi scan (70 to 80% approximately).
Nuclear medicine imaging of myocardial viability & its practical implication