CASES OF THE WEEK – “131-MIBG Scintigraphy In Pheochromocytoma” by Dr ShekharShikare, Consultant & HOD, Nuclear Medicine
131-MIBG SCINTIGRAPHY IN PHEOCHROMOCYTOMA - (SHORT CASE)
Pheochromocytomas (PH or PCC) are rare adrenal tumors arising from chromaffin cells of the adrenal medulla. They make, store, metabolize and usually but not always release catecholamines. Extra adrenal paragangliomas (often described as extra-adrenal pheochromocytomas) are closely related, though less common, tumors that originate in the ganglia of the sympathetic nervous system and are named based upon the primary anatomical site of origin. Pheochromocytomas occur most often during young-adult to mid-adult life.
The diagnosis can be established by measuring catecholamines and metanephrines in plasma (blood) or through a 24-hour urine collection. Imaging by computed tomography or a T2 weighted MRI of the head, neck, and chest, and abdomen can help localize the tumor. Tumors can also be located using an 131-MIBG scan, which is scintigraphy using 131-MIBG -marked metaiodobenzylguanidine.
Testing prior to tumor excision helps ascertain whether the tumor is a singular tumor or if there are multiple, if it is ectopic or adrenal originating, malignant or benign, and isolated or present with other tumors in context of inherited disease. CT is the most commonly used imaging technique; however MRI is preferred. 131-MIBG scanning should be used when possible, as it is the most accurate way to locate catecholamine producing tumors, as catecholamine plasma membrane and vesicular transport systems are especially abundant in pheochromocytoma cells. Imaging using 131-MIBG would yield specific and sensitive results compared to CT and MRI, as the latter two are non-specific generalized imaging techniques
Tumor location
In adults, approximately 80% of pheochromocytomas are unilateral and solitary, 10% are bilateral, and 10% are extra-adrenal. In children, a quarter of tumors are bilateral, and an additional quarter are extra-adrenal. Solitary lesions inexplicably favor the right side. Although pheochromocytomas may grow to large size (>3kg), most weigh <100g and are <10cm in diameter. Pheochromocytomas are highly vascular.
Extra-adrenal pheochromocytomas: Extra-adrenal pheochromocytomas usually weigh 20 to 40g and are <5cm in diameter. Most are located within the abdomen in association with the celiac, superior mesenteric, and inferior mesenteric ganglia and theorgan of Zuckerkandl. Approximately 10% are in the thorax, 1% are within the urinary bladder, and less than 3% are in the neck, usually in association with the sympathetic ganglia or the extracranial branches of the ninth cranial nerves.
Treatment
Surgical resection of the tumor is the treatment of first choice, either by open laparotomy or laparoscopy. Given the complexity of perioperative management, and the potential for catastrophic intra and postoperative complications, such surgery should be performed only at centers experienced in the management of this disorder. In addition to the surgical expertise that such centers can provide, they will also have the necessary endocrine and anesthesia resources. It may also be necessary to carry out adrenalectomy, a complete surgical removal of the affected adrenal gland(s).
Case
25 years old lady apparently ok till four months back. While in sleep, she wakes with sudden onset of headache, forceful pulse, chest pain, and feeling of vomiting (symptoms were progressive with each attack). Similar kind of episode during the daytime (lesser intensity). It has happened 6-7 times in last four months. Each time she went to ER department, she was in hypertensive crisis (220/110 mm of hg) and treated with antihypertensive Rx and sent her home. History of borderline obesity, diabetes mallitus & anaemia.
Ref. To cardiologist for evaluation of HTN → admitted with c/o chest pain and dyspnea with markedly elevated BP → stabilized → work up for secondary HTN → ref to endocrinologist with suspicion of adrenal gland abnormality.
URINE- Sp. Gravity >1.030 (1.003-1.030), PH 5.6 (4.5-7.5), Protein 3+, Blood ++, CRP 10.2 (0.0-5.0), Hemoglobin103 (115-160), MCV 71.3 (78-98), MC hemoglobulin 22.9 (26.5-33.5) Anisocytosis+/ Microcytic+/ Hypochromia+/ Polychromasia+ Mild Microcytic Anaemia.
CARDIAC PROFILE : AST (ASPARTATE AMINOTRANSFERASE) 49 (0-31), CK 81 (0-142), LDH 344 (240-480) CKMB 2.23 (0.00-4.94), TROPNIN T 0.07 (0.01-0.04)
METHOXYLATED CATECHOLAMINE DERIVATIVES
| Nor-metadrenaline | 11088 nmol/24 hours (750-2000) |
| Meta-adrenaline | 698 nmol/24 hours (250-1200) |
| 3 Ortho Methyl dopamine | 2307 nmol/24 hours (600-1300) |
MRI AND MRA- AXIAL AND CORONAL T1w AND T2w IMAGES INCLUDING FAT SUPPRESSION
Both kidney normal in size, shape and position. Both adrenals glands are well defined With body and both limbs are normal in size, shape and signal characteristics Bilaterally. No evidence of adenoma or other focal abnormalities.
MRA RENAL
Right and left kidney is supplied by one prominent artery,both normal in caliber And appearance from aorta. No evidence of any stenosis and signals are Unremarkable.
Ref. for I-131 MIBG WHOLE BODY SCINTIGRAPHY TO LOOK FOR ANY EXTRA-ADRENAL SUSPECTED PHEOCHROMOCYTOMA
131-MIBG whole body images showed well defined focal area of abnormal MIBG accumulation in right adrenal gland as compared to opposite side and the intensity of tracer uptake is more than the liver suggesting metabolically active pheochromocytoma.
On follow up MRI shows about 2 CMS sized well defined right adrenal pheochromocytoma.
Conclusion
MRI is emerging as the technique of choice for the diagnosis of pheochromocytomas, given its ability to safely detect the lesions and differentiate them from adrenal adenomas. In cases of suspected extraadrenal pheochromocytoma, a combination of biochemical tests, MIBG scintigraphy, and MRI may be useful for detection and characterization of such lesions.
Currently, the principle methods of localizations are scintigraphy using 131-MIBG and CT.
CT provides excellent images of the adrenal gland. its sensitivity for detection of the pheochromocytoma is high, since approximately 90% lie within the adrenal gland.
However CT does not differentiate pheochromocytoma, such as cortical adenoma, carcinomas and metastatic disease and it is less sensitive for the detection of extra-adrenal involvement.
Neither the CT/MRI defines the functional nature of the adrenal disorders.
Case 1 - Right pheochromocytoma
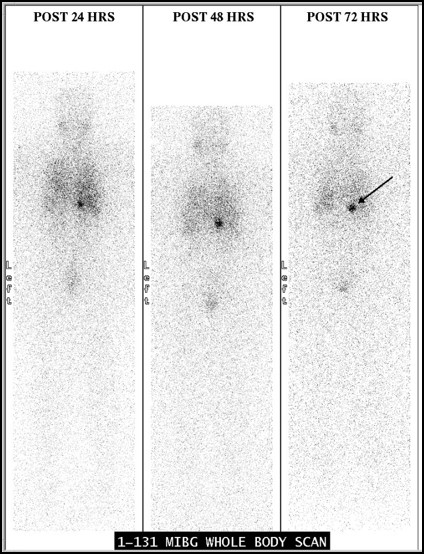
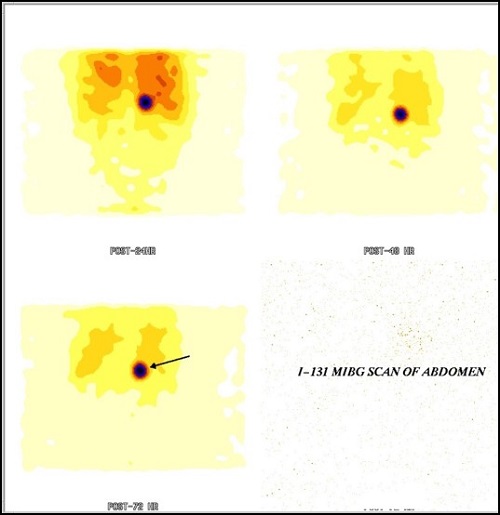
131-MIBG WHOLE BODY IMAGES showed well defined focal area of abnormal MIBG accumulation in right adrenal gland as compared to opposite side and the intensity of tracer uptake is more than the liver suggesting metabolically active pheochromocytoma.
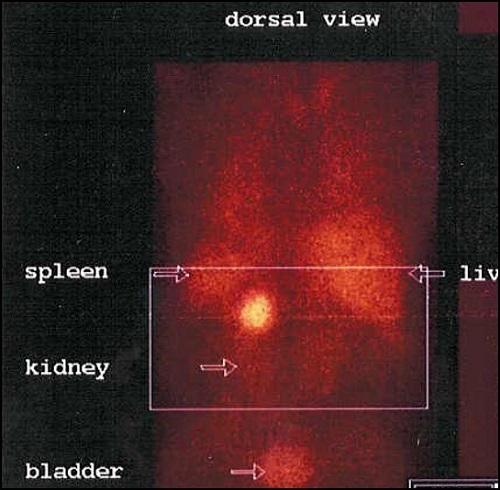
Case 2 - Left pheochromocytoma