CASE OF THE WEEK – “The role of bone scintigraphy in diagnosing reflex sympathetic dystrophy (RSD)” by Dr Shekhar Shikare, HOD & Consultant, Nuclear Medicine, NMC Royal Hospital Sharjah (02)
The role of bone scintigraphy in diagnosing reflex sympathetic dystrophy (RSD)
Introduction
Reflex sympathetic dystrophy (RSD), more recently known as complex regional pain syndrome type I (CRPSI), often presents with pain, swelling, vasomotor disturbance, dystrophic skin changes and motor abnormalities. For patients with these classical findings of RSD, the diagnosis can be made with reasonable confidence. However, not all patients have all these typical findings of CRPSI. Furthermore, the condition progresses through stages – from acute, to dystrophic and atrophic – with many patients experiencing a change in the quality of their pain while, unfortunately, the affected limb develops contractures. The findings of CRPSI may be confused with arthritis, radiculopathy, plexopathy, neuropathy and other less commonly encountered pathologies. Some patients may suffer from two or more of the conditions. The diagnosis of CRPSI may be problematic in the patient who also suffers from diabetic neuropathy. For many patients, treatment of CRPSI with steroids etc.
The CRPS is associated with pro-inflammatory states in the blood, blister fluids, and cerebrospinal fluid. The CRPS-related inflammation may change the sympathetic tone of blood vessels and, therefore, affect blood supply and tissue oxygenation. The acute and chronic phases of CRPS demonstrate different inflammatory features in both clinical manifestations and inflammatory profiles.
Currently, there are no specific pathologic, histologic, or biochemical markers for CRPS 1.However, there is increasing evidence to show that inflammatory processes and immune reactions are involved in the pathophysiology of CRPS.
Several diagnostic procedures, such as bone scintigraphy, plain radiographs, quantitative sensory testing, skin temperature measurements, and fMRI are used to support the diagnosis of CRPS.
Plain radiography is only 60% sensitive and not specific; when radiographs are positive,they often show only osteoporosis, occasionally in combination with soft tissue swelling or diffuse soft tissue atrophy. Plain radiographs of the affected limb can rule out any localized pathology to the bones, joints, and surrounding tissue.Although osteoporosis isfound in as many as 60% of patients with upper extremity reflex sympathetic dystrophy (RSD), it is not specific, often representing changes of disuse secondary to the pain associated with CRPS 1. Occasionally, soft tissue swelling, or diffuse soft tissue atrophy may be seen; these are nonspecific findings.
Radionuclide bone imaging (RNBI) is the only generally accepted imaging technique to provide objective and relatively specific evidence of CRPS 1 in the upper and lower extremities, predominantly the hands and feet.Delayed bone imaging has been reported to be up to 100% sensitive for the variant of sympathetically maintained pain termed RSD by hand and foot surgeons.
Case
25 years old gentleman, who continues to complain of pain in right hand and wrist following an injury to that site.
Blood pool and bone phase-
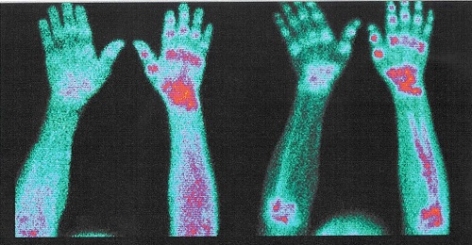
Figure shows - 99mTc-MDP Bone Scintigraphy of The Hands
Blood pool and bone phase of the hands- Abnormally increased tracer uptakes in multiple hand Joints, wrist right hand and even shaft of radius and ulnar bone of right forearm.
Reflex sympathetic dystrophy of the right hand.
Teaching
The RSD is easily recognized when it involves multiple joints of hands or leg, all of which all of which would be covered a by a long glove or stocking.



