CASE OF THE WEEK – “Bone scintigraphy in shin splints, Scintigraphy stress fracture patterns & classification of medial tibial stress syndrome” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine, Dr Osama Batal, Consultant, Orthopaedic Surgery & Dr Mohamed Fahmy, Consultant, Orthopaedic Surgery, NMC Royal Hospital Sharjah
A clinical classification for chronic medial tibial stress syndrome. has been reported to be either tibial stress fracture or microfracture, tibial periostitis, or distal deep posterior chronic compartment syndrome.
Three chronic types exist and may coexist:
Type I (tibial microfracture, bone stress reaction or cortical fracture); type II (peri-ostealgia from chronic avulsion of the periosteum at the periosteal-fascial junction); and type III (chronic compartment syndrome syndrome).
Shin splints (medial tibial stress syndrome) is an inflammation of the muscles, tendons, and bone tissue around the tibia. Pain typically occurs along the inner border of the tibia, where muscles attach to the bone. Shin splint pain most Posterior shin splints are generally caused by imbalances in the leg and foot. Muscle imbalances from tight calf muscles can cause this condition. Imbalances in foot alignment, such as having flat arches (called pronation), can also cause posterior shin splints. often occurs on the inside edge of your tibia (shin bone). Figure 1,2.3
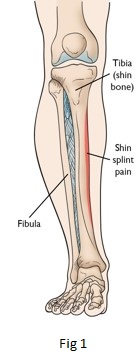
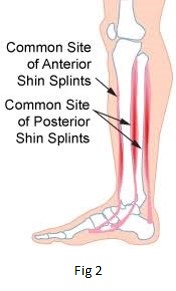
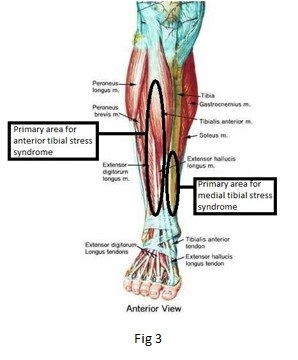
Anterior shin splints are located on the front (or anterior) part of the shinbone and involve the tibialis anterior muscle. The tibialis anterior lifts and lowers your foot. It lifts your foot during the swing phase of a stride. Then, it slowly lowers your foot to prepare your foot for the support phase. (figure 2,3)
Bone scintigraphy Stress fracture patterns were classified into four grades of bone response according to dimension, bone extension, and tracer concentration in the lesions
Grade I: Small, ill-defined lesion with mildly increased activity in the cortical region.
Grade II: Larger than grade I, well-defined, elongated lesion with moderately increased activity in the cortical region.
Grade III: Wide fusiform lesion with highly increased activity in the cortico-medullary region.
Grade IV: Wide extensive lesion with intensely increased activity in the transcortical-medullary region.
Bone scintigraphy patterns have been introduced for distinguishing inflammatory shin-splints from stress fractures, allowing for their appropriate early treatment. Thus, early recognition of mild stress fracture scintigraphy patterns representing the beginning of pathologic bone response to stress enabled a prompt and effective treatment to prevent progression of lesions, protracted disability, and complications.
Case 1
28 years old gentleman complaining of ache and discomfort with severe leg pain during running for the last nine months. It is getting worse recently, causing difficulty in running or even walking for long distances. He has been trying different sorts of non-steroidal anti-inflammatory medication but no avail.
x-ray leg shows no obvious bony abnormality.
Suspected bilateral calf muscle pain with swelling possible stress fracture or chronic compartment syndrome.
Ref for isotope bone scan
99mTc- MDP bone scan of legs (Blood pool, static planar and SPECT CT fused images of the legs)
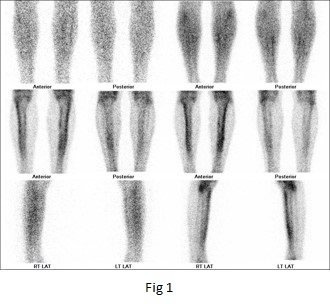
Fig 1- Blood pool and bone images of the legs
Blood pool images shows no obvious abnormal pooling of the tracer.
Fig 1,2,3,4 Static spot bone and SPECT-CT fused images of the legs
It shows abnormal linear shaped increased tracer uptakes in a) Anterolateral cortex of the both the tibial bones inlvoing upper 2/3rd length of the bone & b) Postero-lateral cortex of both the tibial bones invlvoing one third length of the bone (lower portion), with varying tracer uptake intensity (left>right).
CONCLUSION
BILATERAL SHIN SPLINTS (LEFT>RIGHT).
BILATERAL ANTERIOR SHIN SPLINT (left>right).
BILATERAL POSTERIOR SHIN SPLINT (left>right).
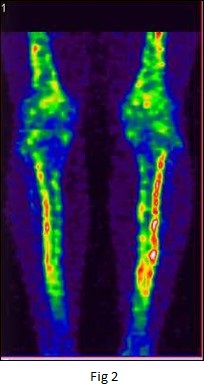
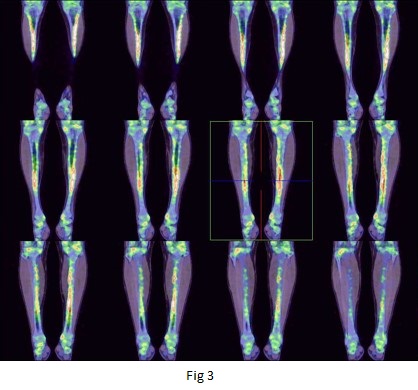
Fig 2 & 3- 3D Images & SPECT CT fused images of legs (anterior view)
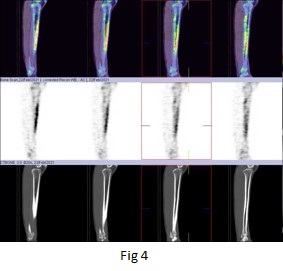
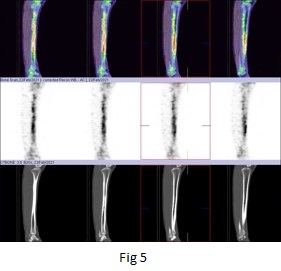
Fig 4 & 5 SPECT-CT fused images of right & left leg (sagittal view)
Case 2
26 years old gentleman complaining of pain in frontal aspect of specially after excericing and after long walking since last one year. No previous hsiotry of trauma both the legs, which is much increased after doing execriscies.
On examination- Severe tense in both the calf region (right>left) even without activity.
Ref for isotope bone scan 99mTc- MDP bone scan of legs (Blood pool, static planar and SPECT CT fused images of the legs)
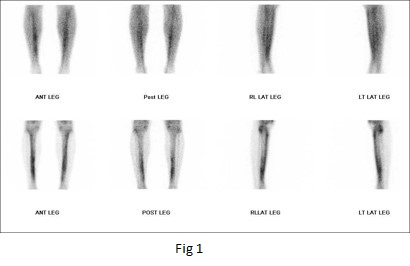
Fig 1- Blood pool and bone images of the legs
Blood pool images shows no obvious abnormal pooling of the tracer.
Fig 1,2,3,4 Static spot bone and SPECT-CT fused images of the legs
It shows abnormal linear shaped increased tracer uptakes in a) Anterolateral cortex of the both the tibial bones inlvoing entire length of the bone & b) Postero-lateral cortex of both the tibial bones invlvoing half of the length of the bone (lower portion).
CONCLUSION
BILATERAL SHIN SPLINTS.
BILATERAL ANTERIOR SHIN SPLINT.
BILATERAL POSTERIOR SHIN SPLINT.
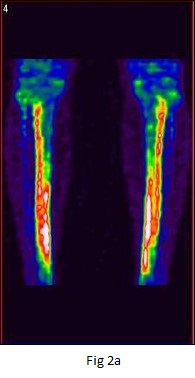
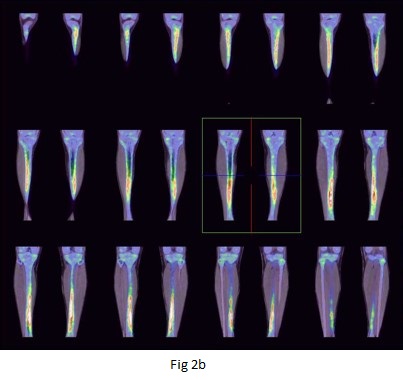
Fig 2a & 2b - 3D Images & SPECT CT fused images of legs (anterior view)
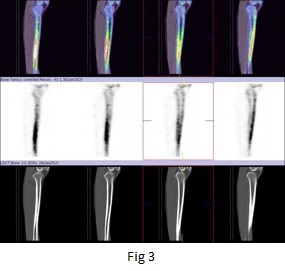
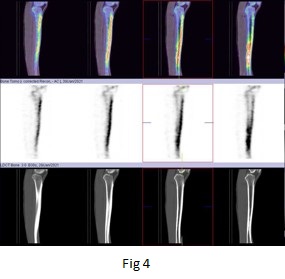
Fig 3 & 4 SPECT-CT fused images of right & left leg (sagittal view).
Discussion
Bone scintigraphy is known to be much more sensitive than radiography for diagnosing shin splints/stress fracture. Early scintigraphy diagnosis, to delineate a scintigraphy classification of stress fractures, and to assess the usefulness of the classification for the management and prognosis of stress fractures and there is distinctive scintigraphy patterns and corresponding disease course of inflammatory shin splints.
Stress fractures and shin splint inflammatory lesions differed. Shin splints appeared as diffuse non focal periosteal uptake, mild in intensity, along the anterolateral border of the tibiae, extending along the proximal two-thirds of the bone shaft.
Stress fractures, on the other hand, were always located along the medial cortex, focal, single or multiple, elongated, fusiform, or transverse areas of increased uptake. No single stress fracture was seen to extend beyond one-third of the cortical bone length and was always located and confined to the medial aspect of the cortex (in Grades I and II) or extended intra medullary to a varying extent (in Grades III and IV).
Shin splints diagnosed clinically, and by bone scintigraphy were treated and responded, mainly to anti-inflammatory drugs, while stress fractures of all grades were treated and responded as verified by bone scintigraphy to rest treatment, with anti-inflammatory drugs having no significant effect.



