Pregnancy and Postpartum Depression


Postpartum Depression is not your fault. It is real; but treatable psychological disorder
World Health Organization (WHO) ranks unipolar depression first in Disability Adjusted Life Years (DALYs) amongst all diseases worldwide for women in their reproductive years
Women present with more:
- Atypical features (Psychomotor retardation, appetite, weight gain)
- Seasonal component
- Higher level of somatic symptoms, ruminations, feelings of worthlessness of guilt
- Higher rates of attempted suicides/lower rates of completed suicides
Pregnancy does not protect against mental illness

Prevalence by Trimester (adult women)
1st trimester 7.4%
2nd trimester 12.8%
3rd trimester 12%
Mean Prevalence in adolescents is 16%
Environmental factors, such as social support and socioeconomic status play a significant role in a person’s lifestyle and mental health status.
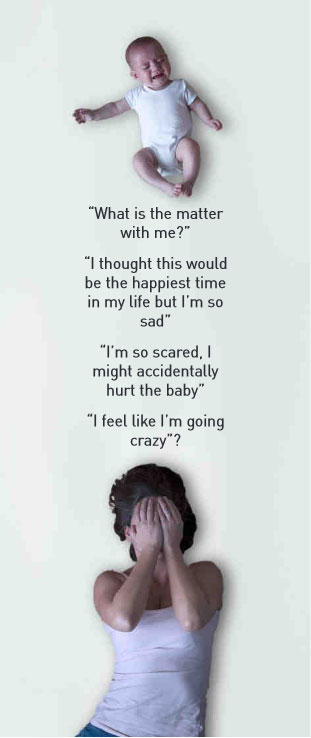
Postpartum depression:

- It is a major depressive episode onset occurs during pregnancy or in the first four weeks following childbirth
- Clinically: Postpartum depression is within 12 months of childbirth
- Women suffering from post-partum depression often reported high levels of parenting stress and low social supports
- Obsessions of child harm, and a range of anxiety disorders all require specific psychological treatments
- A loss of pleasure or interest in things you used to enjoy, including sex
- Eating much more or much less than you usually do
- Anxiety – all or most of the time – or panic attacks
- Racing, scary thoughts
- Feeling guilty or worthless – blaming yourself
- Excessive irritability, anger or agitation – mood swings
- Sadness, crying uncontrollably for very long periods of time
- Fear of not being a good mother
- Fear of being left alone with the baby
- Misery
- Inability to sleep, sleeping too much, difficulty falling or staying asleep
- Disinterest in the baby, family and friends
- Difficulty concentrating, remembering details, or making decisions
- Thoughts of hurting yourself or the baby (see inside this brochure for
- Numbers to call to get immediate help). If these warning signs or symptoms
- Last longer than 2 weeks, you may need to get help.
Whether your symptoms are mild or severe, recovery is possible with proper treatment.
Prevalence
- 10 – 22% of adult women
- 26% of adolescent mothers
- Rates reported from 40 – 53 % in adolescent mothers
- 60% of women have their first depressive episode in the postpartum period
Postpartum Blues

- Prevalence 50 – 85%
- As many as 25% of these women are at risk for development of postpartum depression within the first year
- Mild and transient
- Symptoms: Low mood, crying, mood lability, irritability, anxiety, insomnia, memory and concentration problems
- Course: begins 3 – 4 days after delivery – peaks at day 5 – 6, back to normal in 2 – 3 weeks
- Mother’s functioning usually preserved.
- Treatment limited to support and reassurance
- Psychosocial Risk Factors for Perinatal Depression
- Lack of partner, family and social support.
- Stressful life events
- Breast feeding difficulties
- Colicky babies / infant health problems
- Unplanned pregnancy
- Socio-economic status
- Abuse issues
- Remission of maternal depression after 3 months of medication Rx was significantly associated with reductions in children’s depressive, anxiety & disruptive behaviour disorders and symptoms



