Minimal Invasive Bariatric Surgery - Patient Handbook

Introduction
The physicians and staff of the Bariatric and Metabolic centre at NMC Royal Hospital wish to extend a warm welcome to you and your family. This information booklet is provided to patients considering surgical treatment for severe obesity. You are highly encouraged to read this booklet prior to your scheduled visit in order to be fully prepared. It is recommended that you and your family review the entire booklet thoroughly. We hope that the answers to most of your questions can be found by reviewing the contents of the booklet. Please feel free to bring any additional questions and ask them at the time of your visit.
Weight loss is more than a surgery

Having bariatric surgery can help you lose a significant amount of weight, but a successful outcome requires a permanent and life-long commitment to a healthy lifestyle. The goal of bariatric surgery is to provide a “tool” to assist you with your weight loss and to decrease the long-term risk of medical complications caused by obesity. It is crucial to adhere to the proper diet and exercise program and to receive psychological support. In addition, working closely with your healthcare team will ensure that your weight loss is safe as well as successful.
What is Obesity?
Obesity is a serious medical condition that can decrease your lifespan. It is a complex medical condition in which excess body fat has accumulated to the extent that it can have an adverse effect on health.
Obesity is commonly measured by using the Body Mass Index, or BMI. It is a measurement of height versus weight and is a reliable indicator of body fat for most people. To determine your BMI, please use the calculator available in many websites.
|
BMI Range |
Body Weight |
|
Under 19 |
Underweight |
|
19-24 |
Ideal |
|
25-29 |
Overweight |
|
30-34 |
Obese, may qualify for weight loss intervention |
|
35-40 |
Morbidly Obese, qualifies for surgery with selected health problem |
|
Over 40 |
Morbidly obese, qualifies for surgery |
Health Effects of Obesity

Individuals affected by severe obesity are often affected by many other obesity-related conditions and diseases, such as type 2 diabetes, hypertension and sleep apnea. Severe obesity can damage the body and affect nearly every organ in the body in some way. Life expectancy decreases as weight increases, especially in the severely obese.
Diabetes: Patients with obesity are more likely to develop diabetes than patients with a healthy BMI. Over time, obese individuals develop resistance to insulin, which regulates blood sugar levels. A diagnosis of Type 2 diabetes is reported to be a major cause for amputations, cardiovascular disease, stroke and blindness. Diabetes can also lead to a number of other complications including kidney disease, hypertension, lipid abnormalities, circulatory and nerve defects, chronic infections, impotence and more.

Cardiovascular Disease: The American Heart Association considers obesity a major risk factor for heart disease such as coronary artery disease, heart attack, enlargement of the left side of the heart which may result in congestive heart failure, in addition, greater incidence of arrhythmias (irregular heartbeats) resulting in a three-fold increased risk of cardiac arrest. Obesity is a major contributor to hypertension (high blood pressure). Obesity puts a strain on the entire circulatory system, increasing the risk for stroke.

Respiratory Disorders: Obesity can reduce respiratory capacities and individuals are more susceptible to respiratory infections, to greater incidence of asthma and the majority have a serious breathing disorder known as obstructive sleep apnea (OSA) which occurs when excess fat in the neck, throat and tongue obstructs air-passage ways during sleep (a temporary cessation of breathing). An OSA episode each night causes exceptionally low oxygen levels in the tissue and blood which may contribute to systemic and pulmonary hypertension, heart failure, sudden cardiac death and stroke, as well as fatigue and drowsiness.
Accidents: Severe obesity contributes to the development of a number of musculo-skeletal issues that increase the risk for accidents, including aggravated joint diseases (osteoarthritis, gout), disc herniation, spinal abnormalities, and pseudo tumour cerebri, a condition associated with disorientation and visual impairment.
Liver Disease: Obesity is the major cause for fatty liver and non-alcoholic fatty liver disease. The majority of individuals with severe obesity have non-alcoholic fatty liver disease. Fatty liver disease can cause progressive fibrosis of the liver, resulting in impaired liver function, and eventually can progress to cirrhosis and liver failure.
Criteria for Bariatric Surgery

To be a candidate for bariatric surgery,
patients should meet all of the criteria below, as established by the international and European standards.
- Have a Body Mass Index (BMI) of 40 or higher – or 35 or more with obesity-related diseases such as Type 2 diabetes, sleep apnea, or high blood pressure
- Have attempted (and failed) previous weight loss efforts with diet, exercise, lifestyle changes, or medications
- 3. You must be knowledgeable about the possible risks, benefits, and side effects of the procedures
- You must understand and be committed to the necessary lifestyle changes
- You should be committed to long-term follow up care.
- You must be treated for any psychiatric or emotional conditions that would prohibit success after surgery
- You must be motivated and have realistic expectations of the surgical outcomes
Bariatric Surgery Overview
- Treatments for obesity include
- Diet
- Behavioural modification
- Exercise
- Medications
- Surgery
- Most severely obese people do not experience successful weight loss with dieting alone.
- The best long-term result for the treatment of morbid obesity is surgical treatment. Options include: Roux- en-Y Gastric Bypass, Sleeve Gastrectomy, and Adjustable Gastric Band.
Roux-en-Y gastric Bypass
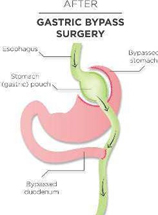
The gastric bypass op- eration is both a restric- tive and malabsorptive procedure. It is designed to limit the amount of food you eat and absorb. This surgery reduces the stomach to the size of an egg and will change the way food passes through the intestine. The small- er opening recreated be- tween the stomach and small intestine slows the rate of the food emptying from the stomach into the small intestine. This increases the feeling of fullness, therefore, helping you to eat less.
Sleeve Gastrectomy

This procedure generates weight loss through gastric restriction (reduced stomach volume) and chemical/hormonal changes. A large proportion of the hormone called Ghrelin, known to control appetite, is located in the part of the stomach that is removed. The stomach is restricted by stapling and dividing it vertically and removing more than 85% of it. The stomach that remains is shaped like a very slim banana. The nerves to the stomach and the outlet valve (pylorus) remain intact with the idea of preserving the functions of the stomach while drastically reducing the volume.
Gastric Lap Band
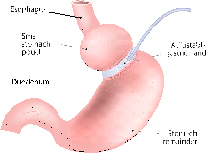
The adjustable gastric band is a restrictive procedure that limits the amount of food that enters the stomach. In this surgery, a hollow band made of silicon is placed around the stomach near its upper end, creating a small pouch and a narrow passage into the larger remainder of the stomach. The band is then inflated with a sterile water solution. It can be tightened or loosened over time to change the size of the passage by increasing or decreasing the amount of sterile water solution. The band is not filled at the time of surgery. The initial adjustment is approximately one month after surgery.
Following Bariatric Surgery: Overview


- After surgery, conditions such as high blood pressure, type 2 diabetes, sleep apnea, and arthritis may improve dramatically, and in many cases, resolve completely.
- A six-month physician-supervised low calorie diet is required.
- Bariatric surgeries involve some risk of complications that could result in intensive care treatment and possible re- operation. The major surgical risks include:
- Blood clots in the lungs
- Leaks
- Obstructions of intestine
- Bleeding
- Strictures
- Death with an average risk of less than 1 out of 1,000 patients (<0.1%), (due to a patient’s health problems or complications from surgery).
- After bariatric surgery, you should eat 3 small meals per day
- After surgery, you cannot eat as much of any kind of food as you want and still lose weight
- Important vitamins and minerals after bariatric surgery may include multivitamins, B12, calcium, iron, and Vitamin D. These supplements help decrease the risk of anaemia (low blood counts) and bone loss or serious nerve or brain problems.
- Weight loss is not guaranteed long-term. Weight regain can occur if you fail to follow all of the guidelines. Follow- up visits will help you keep the weight off
- Average weight loss at one year after surgery is about 70% of excess body weight, though 1 out of 10 patients will lose almost all of their excess weight.
- You are encouraged to begin exercising soon after surgery and maintain an exercise program to achieve better weight loss outcomes.
- Dumping Syndrome describes the side effects which occur after eating too much sugar or greasy foods for those patients who had a gastric bypass or sleeve surgery. You may feel light-headed, nauseated, experience palpitations, and feel sweaty a few minutes after consuming foods that are high in sugar or fat
- Females of child-bearing age should wait at least 18 months after surgery before becoming pregnant to decrease the potential risk of nutritional problems for both the mother and the foetus
- If you are experiencing any problems related to your surgery (including nausea, abdominal pain, difficulty tolerating foods), you should call your surgeon’s office
- Certain pain medications, including aspirin and ibuprofen should be avoided after surgery. NSAIDs can cause stomach ulcers especially in gastric bypass patients. Acid reducer medications must be used in conjunction with any NSAID intake



