Hemorrhoids
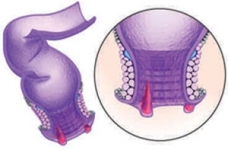

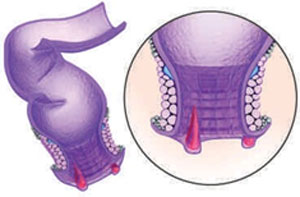
Hemorrhoids also called piles, are swollen veins in your anus and lower rectum, similar to varicose veins. Hemorrhoids have a number of causes, although often the cause is unknown. They may result from straining during bowel movements or from the increased pressure on these veins during pregnancy. Hemorrhoids may be located inside the rectum (internal hemorrhoids), or they may develop under the skin around the anus (external hemorrhoids).
Hemorrhoids are very common. Nearly three out of four adults will have hemorrhoids from time to time. Sometimes they don’t cause symptoms but at other times they cause itching, discomfort and bleeding.
Occasionally, a clot may form in a hemorrhoid (thrombosed hemorrhoid). These are not dangerous but can be extremely painful and sometimes need to be lanced and drained.
Fortunately, many effective options are available to treat hemorrhoids. Many people can get relief from symptoms with home treatments and lifestyle changes.
Symptoms
Signs and symptoms of hemorrhoids may include:
- Painless bleeding during bowel movements — you might notice small amounts of bright red blood on your toilet tissue or in the toilet
- Itching or irritation in your anal region
- Pain or discomfort
- Swelling around your anus
- A lump near your anus, which may be sensitive or painful (may be a thrombosed hemorrhoid)
Hemorrhoid symptoms usually depend on the location.
Internal hemorrhoids:
These lie inside the rectum. You usually can’t see or feel these hemorrhoids, and they rarely cause discomfort. But straining or irritation when passing stool can damage a hemorrhoid’s surface and cause it to bleed.
Occasionally, straining can push an internal hemorrhoid through the anal opening. This is known as a protruding or prolapsed hemorrhoid and can cause pain and irritation.
External hemorrhoids:
These are under the skin around your anus. When irritated, external hemorrhoids can itch or bleed.
Thrombosed hemorrhoids:
Sometimes blood may pool in an external hemorrhoid and form a clot (thrombus) that can result in severe pain, swelling, inflammation and a hard lump near your anus.
When to see a doctor
Bleeding during bowel movements is the most common sign of hemorrhoids. Your doctor can do a physical examination and perform other tests to confirm hemorrhoids and rule out more-serious conditions or diseases.

Also talk to your doctor if you know you have hemorrhoids and they cause pain, bleed frequently or excessively, or don’t improve with home remedies.
Don’t assume rectal bleeding is due to hemorrhoids, especially if you are over 40 years old. Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer. If you have bleeding along with a marked change in bowel habits or if your stools change in color or consistency, consult your doctor. These types of stools can signal more extensive bleeding elsewhere in your digestive tract.
Seek emergency care if you experience large amounts of rectal bleeding, lightheadedness, dizziness or faintness.
Causes
The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from increased pressure in the lower rectum due to:
- Straining during bowel movements
- Sitting for long periods of time on the toilet
- Chronic diarrhea or constipation
- Obesity
- Pregnancy
- Anal intercourse
- Low-fiber diet
Hemorrhoids are more likely with aging because the tissues that support the veins in your rectum and anus can weaken and stretch.
Complications
Complications of hemorrhoids are very rare but include:
- Anemia. Rarely, chronic blood loss from hemorrhoids may cause anemia, in which you don’t have enough healthy red blood cells to carry oxygen to your cells.
- Strangulated hemorrhoid. If the blood supply to an internal hemorrhoid is cut off, the hemorrhoid may be “strangulated,” another cause of extreme pain.
Prevention
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can cause hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Drink plenty of fluids. Drink six to eight glasses of water and other liquids (not alcohol) each day to help keep stools soft.
- Consider fiber supplements. Most people don’t get enough of the recommended amount of fiber - 25 grams a day for women and 38 grams a day for men - in their diet. Studies have shown that over-the-counter fiber supplements, such as Metamucil and Citrucel, improve overall symptoms and bleeding from hemorrhoids. These products help keep stools soft and regular.
If you use fiber supplements, be sure to drink at least eight glasses of water or other fluids every day. Otherwise, the supplements can cause constipation or make constipation worse.
- Don’t strain. Straining and holding your breath when trying to pass a stool creates greater pressure in the veins in the lower rectum.
- Go as soon as you feel the urge. If you wait to pass a bowel movement and the urge goes away, your stool could become dry and be harder to pass.
- Exercise. Stay active to help prevent constipation and to reduce pressure on veins, which can occur with long periods of standing or sitting. Exercise can also help you lose excess weight that may be contributing to your hemorrhoids.
- Avoid long periods of sitting. Sitting too long, particularly on the toilet, can increase the pressure on the veins in the anus



